Whenever a patient is being discharged from a hospital or in a health care center, it means that the patient’s condition has been improved and his or her health is already back to normal. However, before the patient will be declared discharged, there is a certain procedure to follow. That procedure is pertaining to the hospital records. The doctors and other health care workers should make sure that the medical care given to the patient is properly recorded. The record itself is the discharge summary report. In this article, you will be able to know more about what a discharge summary report is.
10+ Discharge Summary Report Samples
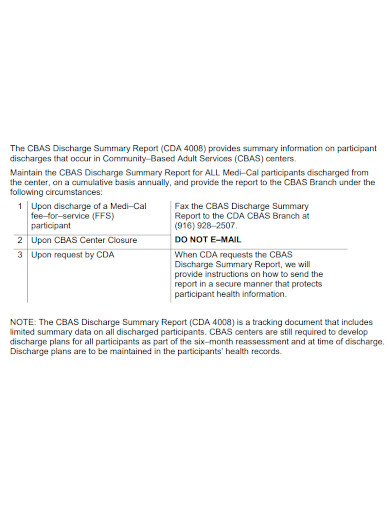
1. Discharge Summary Report
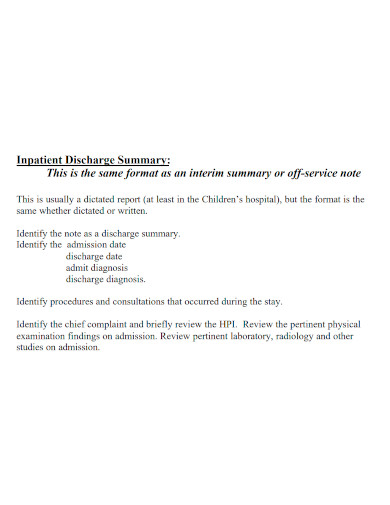
2. Timely Discharge Summary Report
3. Electronic Discharge Summary Report
4. Discharge Summary Report Form
5. Discharge Summary Report Format
6. Standard Discharge Summary Report
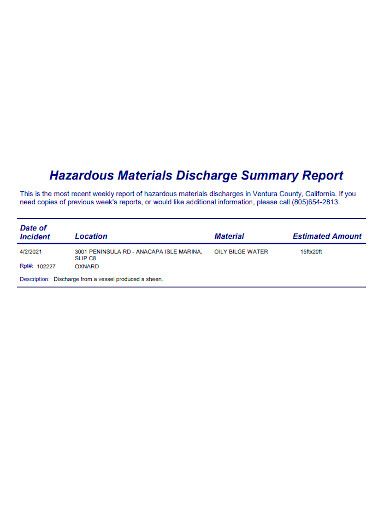
7. Hazardous Materials Discharge Summary Report
8. Editable Discharge Summary Report
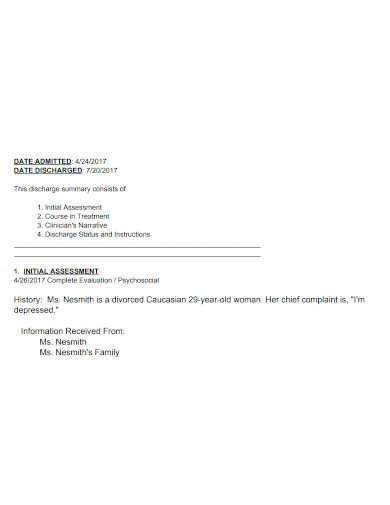
9. Patient Discharge Summary Report
10. Professional Discharge Summary Report
11. Printable Discharge Summary Report
What is a Discharge Summary Report?
A discharge summary report is a type of document that is essential for transferring information between the attending physician and the patient. However, summaries often have insufficient information and would fail to reach for the attending physician in case there will be a follow-up visit or check-up.
Taken from a literature published in the year 2007 entitled Journal of the American Medical Association (JAMA), states that some information or data in the discharge summaries were missing like in the case of medications at discharge that did not appeared on the list, omitted diagnosis and pending results from laboratory tests. Some studies also found out that there are some discharge summaries that were not sent to the outpatient provider. Discharge summaries also suffer from being too lengthy containing unimportant information.
A structured discharge summary report ensures that all necessary information will be included and allows all attending physicians to easily identify the right method as to how to respond to a particular patient’s hospitalization.
Components of a Discharge Summary Report
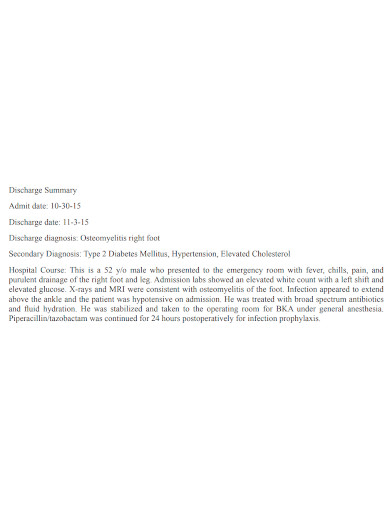
A structured discharge summary is very essential in transferring information between the hospital and aftercare providers, promoting patient safety, for legal purposes and in helping attending physicians to respond quickly about the patient’s hospitalization. The discharge report must contain the findings, laboratory test results, and more.
Below are the components that should be included in the discharge summary report:
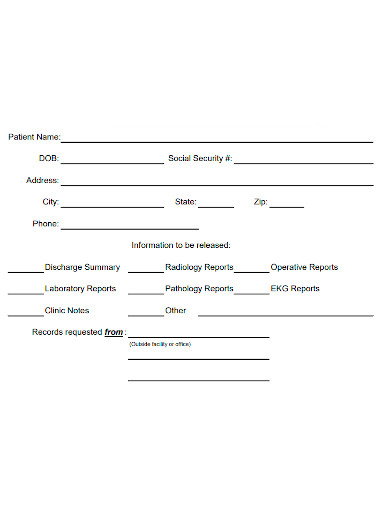
1. Reason for patient’s hospitalization – this must contain information about the patient’s condition, and the history of the illness.
2. Findings or diagnosis – this refers to the information about the primary diagnoses in both admission and discharge
3. Procedures and treatment – procedures and treatment refers to the events that occurred during the patient’s stay in the hospital, hospital consults and procedures.
4. Patient’s discharge condition – this refers to the documentation of the health and condition status of the patient during discharge.
5. Patient and family instructions – this contains the list of the discharge medications, activity orders or the patient’s activity level upon discharge, therapy orders that can be either physical or occupational, follow-up plans such as appointment dates or timeframe for the next follow-up, and dietary instructions for the patient’s recommended food intake.
6. Attending physician’s signature – this can be either electronic or physical signature
FAQs
Why do we need to keep the discharge summary short?
It is best to keep the summary short so that it would be readable and would only contain information that are relevant for the attending physician.
What is the purpose of discharge summary report?
The purpose of a discharge summary report is to provide communication that accompanies a patient to his or her next setting care.
What do you mean by discharge diagnosis?
A discharge diagnosis is considered as the final diagnosis given before a patient will be released in the hospital.
Discharging a patient requires a lot of complex procedures and could be one of the most essential part in the creation of a discharge plan. Generally, discharge summary report is used to be able to have a communication between the health care providers, the aftercare and the patient. However, if the physician makes errors while making the report, it could jeopardize the process.
Related Posts
FREE 10+ Summary Writing Samples
FREE 10+ Validation Report Samples
FREE 9+ Sample Occupational Therapy Job Descriptions
FREE 9+ Medical Records Clerk Job Description Samples
FREE 8+ Sample Dental Records
FREE 8+ Sample Medical Reports
FREE 8+ Patient Note Samples
FREE 8+ Mental Health Counselor Job Descriptions
FREE 7+ Sample Psychological Evaluations
FREE 5+ Medical Records Manager Job Descriptions
FREE 11+ Medical Bill Receipt Templates
FREE 11+ One-Page Writing Samples
FREE 10+ Radiologist Job Description Samples
FREE 9+ Sample Employee Counseling Forms
FREE 9+ Sample Hospital Organizational Chart Templates