A discharge summary is an important document to help keep the patient safe and in a stable and good condition when they are discharged from the hospital. It tells them the diagnosis of their health problem, the treatment they received, and the medications and ongoing treatment they need to take after being discharged. Physicians are responsible to give the instructions while nurses are the ones responsible to transcribe the details in the discharge summary note. Making a discharge summary is easy, as long as you already have the important details to input in the summary. Read the article to know how to make a discharge summary nursing note.
5+ Discharge Summary Nursing Note Samples
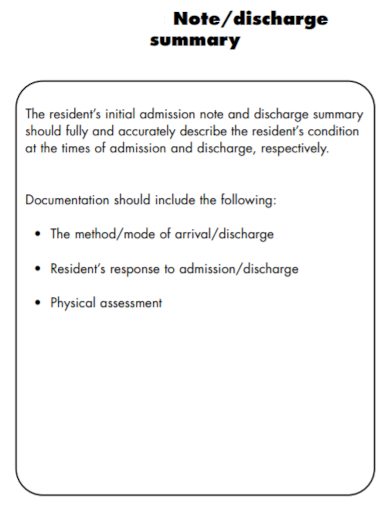
1. Discharge Summary Residential Nursing Note
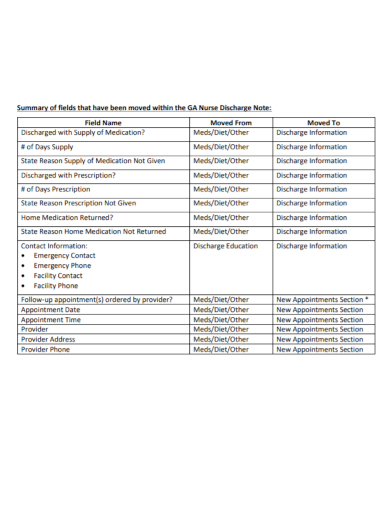
2. Discharge Summary Nursing Field Note
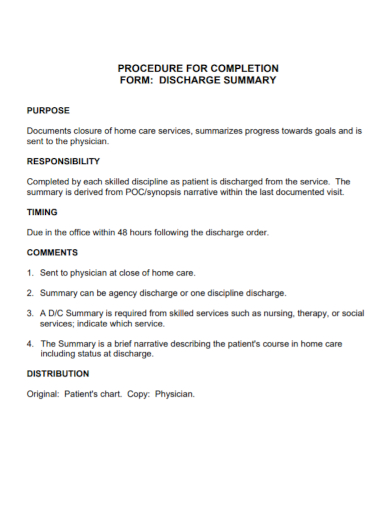
3. Discharge Summary Nursing Procedure Note
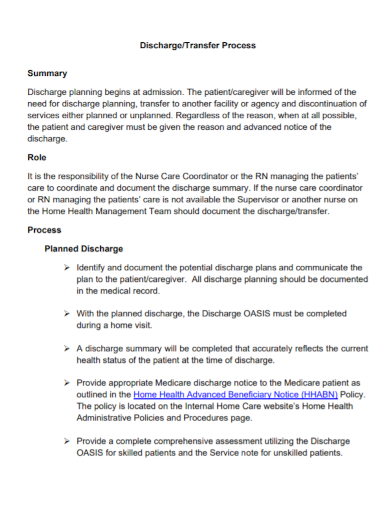
4. Discharge Summary Nursing Transfer Note
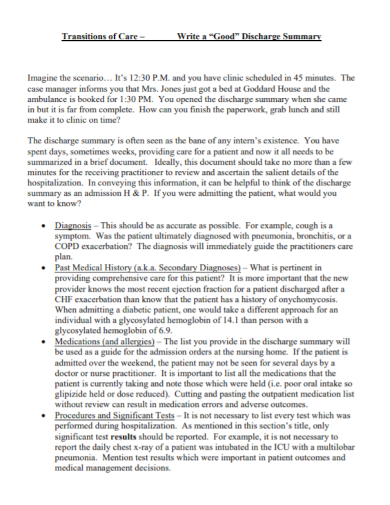
5. Discharge Summary Transitions Care Note
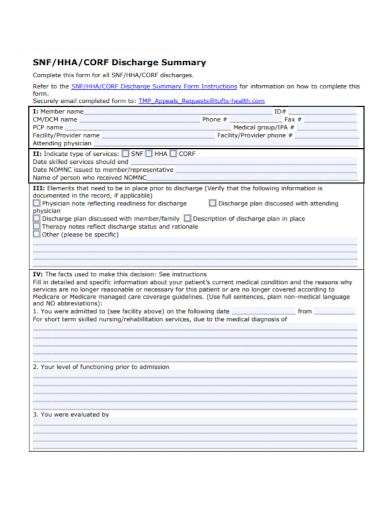
6. Discharge Summary Physician Note
What is a Discharge Summary?
A discharge summary is a letter written by the physician who is assigned to take care of a patient admitted to the hospital and is going to be discharged soon. It contains important information about the patient’s hospital visit. The summary is printed in several copies for the patient’s copy, the physician, and the hospital for record-keeping.
Details to Include in a Discharge Summary Nursing Note
1. Patient Details
The first part of the summary note is the patient’s details. Important information must be included about the patient like personal information and emergency contacts.
2. Hospitalization Reasons
The next part of the summary is the description of the patient’s primary present condition and the patient’s initial diagnostic evaluation.
3. Findings
The next part is the findings or the diagnoses that the attending physician made during the patient’s stay in the hospital. When documenting the diagnoses, make sure the details are specific. If no diagnoses are being made, document the present complaint of the patient and explain that no cause was identified.
4. Procedures and Treatment
This part is where you include the information on how the patient was treated during their stay. The information must include:
- Management: Explain how the patient was managed during their hospital stay (include any long-term management, if it’s the case for the patient) and description of the events that occurred to the patient during their stay.
- Complications: Include details of any complications that happened
- Procedures: This part must include all medical procedures (such as operations, for example) that the patient underwent. Give a comprehensive explanation here such as the date of procedure, the procedure itself; such as the surgery process, any anesthesia agents being injected into the patient, etc.
5. Discharge Condition of the Patient
Document how the patient is doing and their health condition while on the way for their discharge.
6. Medical Instructions
The next part is the instructions from the physician to the patient and their family. The details here must include their discharge medication, activity and therapy orders, dietary instructions, medical follow-up, and treatment for chronic illnesses.
7. Physician’s signature
The summary must be concluded with the signature of the attending physician on the discharge summary.
FAQs
Why is a discharge summary important?
A discharge summary is important because it describes your whole experience, diagnosis, and treatment you had from your hospital visit and also informs your physician regarding the details above and the prescription given to you by your attending physician from the hospital for them to review it and recommend you other forms of treatment or medication or advise you to continue the hospital’s instructions.
Is a discharge summary required?
A discharge summary is a common protocol for all discharged patients in every hospital so it is required.
How do you know if a patient is ready for discharge?
Physicians and nurses observe patients throughout their stay in the hospital. They know when a patient is ready to be discharged when the patient has a tolerance of oral intake medicine, can move by themselves and do self-care independently, and that they are healing from surgery (or illnesses) without complications.
If you are in charge to transcribe all the doctor’s and nurse’s discharge notes, make sure you include every specific detail. Make sure that no important detail is forgotten. Always review the summary before sending it to the physician for review. To help you get started writing the discharge summary nursing note, download the free sample templates provided above to use as your guide.
Related Posts
FREE 9+ Medical Records Clerk Job Description Samples
FREE 9+ Sample Employee Counseling Forms
FREE 9+ Sample Hospital Organizational Chart
FREE 8+ Sample Professional Summary
FREE 7+ Sample Contract Summary
FREE 7+ Sample Physical Therapy Evaluations
FREE 20+ Medical Report Templates
FREE 11+ Sample Discharge Summary
FREE 11+ Nursing Care Plan Templates
FREE 10+ Summary Writing Samples
FREE 9+ Sample Occupational Therapy Job Description
FREE 8+ Sample Business Summary
FREE 8+ Sample Psychiatrist Job Description
FREE 7+ Sample Discharge Summary
FREE 7+ Doctor Receipt Templates