Everything that we are about to do in health care should be done through an informed consent. Every patient should know about the procedures that health care providers do to them so they can fully understand the benefits, risk, and the alternatives. Health care process would really require an extensive informed consent discussion especially a documentation of a specific procedure note. If we think that a certain intervention is essential, always make it clear to the patient why we should take that certain procedure. If they decline, it should also be stated to the medical record the reason why. In this article, you are going to know more about procedure note and its contents.
10+ Procedure Note Samples
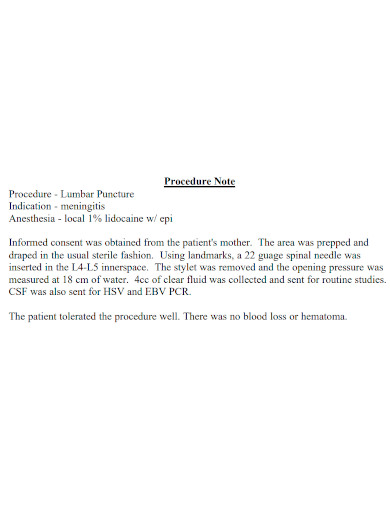
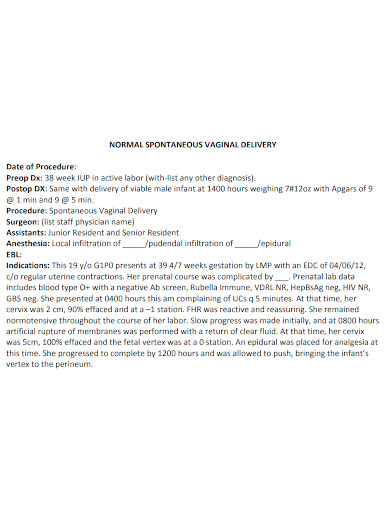
1. Procedure Note Sample
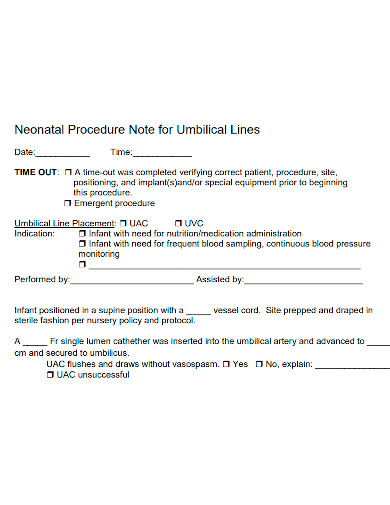
2. Neonatal Procedure Note
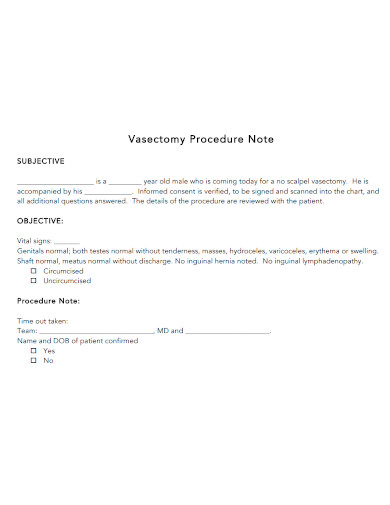
3. Vasectomy Procedure Note
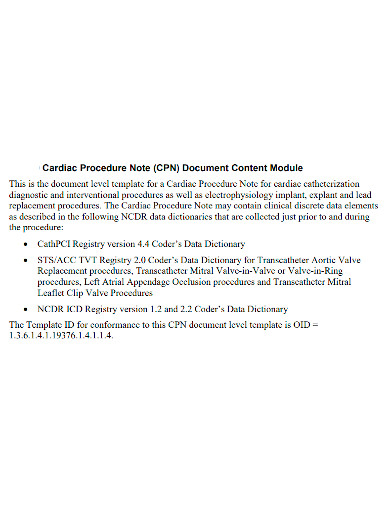
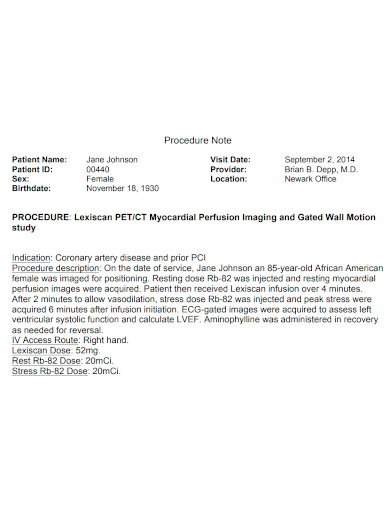
4. Cardiac Procedure Note
5. Procedure Note Format
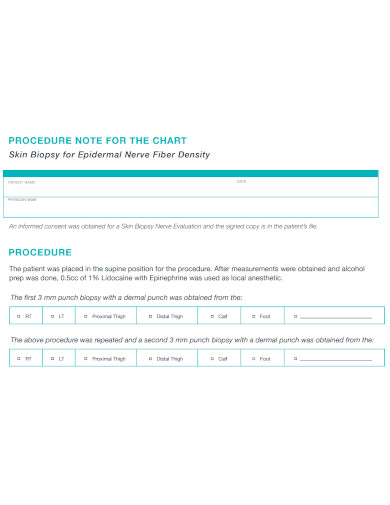
6. Chart Procedure Note
7. Printable Procedure Note
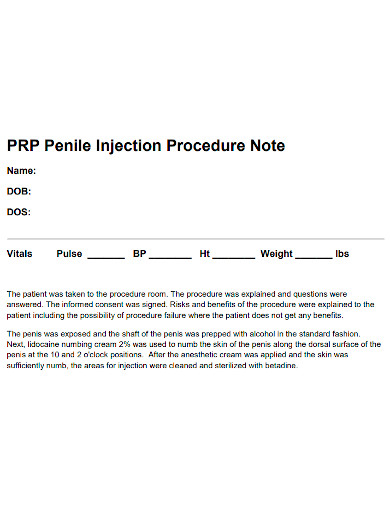
8. Penile Procedure Note
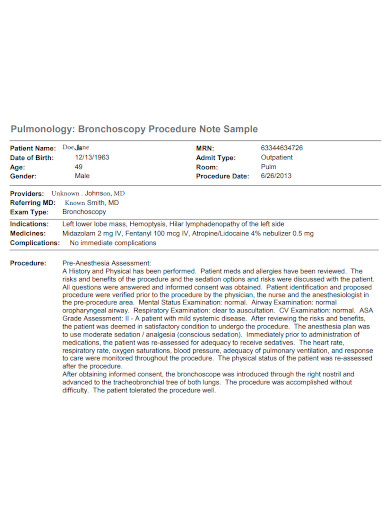
9. Bronchoscopy Procedure Note
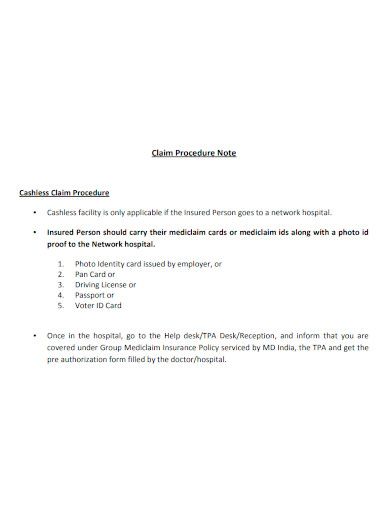
10. Claim Procedure Note
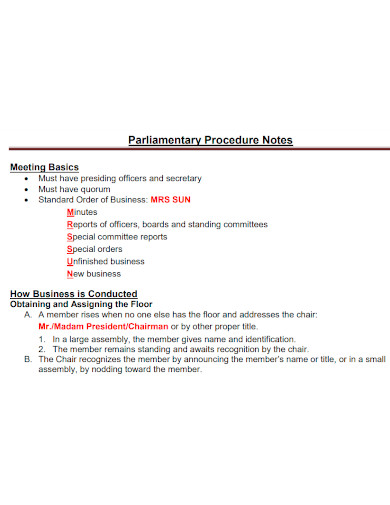
11. Parliamentary Procedure Note
What is a Procedure Note?
A procedure note is considered as the largest section of the OP report wherein there will be a physical document of the specifics about what a physician did. The outline should be able to provide the details including patient position, approach, depth, anatomic site, findings. Physicians do not necessarily specify what approach they used. They can even document any type of complications as well as abnormal findings. They also document details like time of the procedure that requires more work. The physician can be able to include in the procedure note the biopsies, lesions, anastomoses, foreign bodies, grafts, blood loss, excisions, hardware used for repair, and tubes for feeding and other purposes. They can also provide report about the type of closure that has enough detail to give support to any additional work.
Example of Procedure Note
Vasectomy Procedure Note
INDICATIONS:
PROCEDURE:
https://www.venturafamilymed.org
FAQs
Does a procedure note requires patient consent?
Yes. It is noted that the patient was given an opportunity to ask questions and consent the procedure.
How should a procedure note be done?
It can be done either in written form or dictated.
What should be included in a procedure note?
It must have the date and time, name of the procedure done, indications, patient’s consent, type of anesthesia used, procedure description, disposition, signature, etc.
Procedure notes should be written or dictated clearly and concisely so that it would be easier to understand. It can also give clarifications to the patients if the texts are recorded correctly. Writing a procedure note should also be following a specific format so that it would be organized and more formal to read. Check out our sample procedure notes!
Related Posts
FREE 14+ Software Test Plan Templates
FREE 13+ Journal Entry Samples
FREE 10+ Therapy Progress Note Samples
FREE 8+ Consignment Note Samples
FREE 7+ Sample Process Manual Templates
FREE 5+ Handover Note Templates
FREE How to Write a Navy Standard Operating Procedure?
FREE Procedure Manual Samples
FREE 38+ Notes Samples
FREE 10+ Administration of Medication Policy Samples
FREE 10+ Employee Attendance Policy Samples
FREE 9+ Sample Progress Note Templates
FREE 8+ Sample Procedure Manuals
FREE 7+ Sample Shipping Manual Templates
FREE 7+ Sample Release Note Templates