A progress note is mainly created and used by doctors , nurses , social workers and health physicians in keeping tabs on the welfare of a patient or client medical wise. The notes provide an easy follow up on a patient’s status and the treatment undertaken. Progress note is an essential part of a medical record as it allows follow ups and pickup on a certain patient by different participating care givers. It’s easy for a different physician to treat a new patient on his list by consulting information the patient’s progress note. Progress notes templates are available in various types for different purposes. In this article we will explore the physicians’ progress notes and when they are used and what their purposes are. You can also see Daily Notes Template
Patient Progress Note Template
Prepared by a healthcare professionals and provider; patient progress notes is more focussed on the medical aspects hence describes the medical condition, the treatments and care to /of a patient. It details a patient clinical tenure that is both progressive and regressive. Progress note template only contains date, patient name and the doctor’s notes.
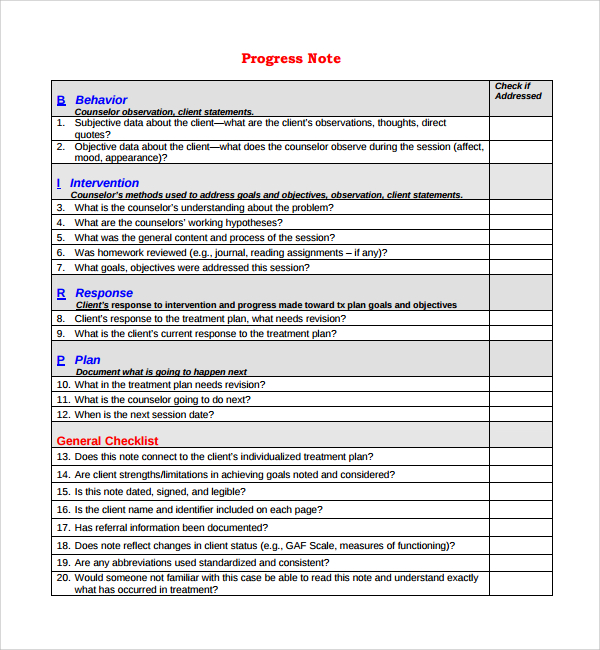
Client Progress Note Template
Client progress notes are written by staff of a company about a specified client. It includes a client’s achievements, status and any other details about a client. Client progress note is aimed at reflecting a client’s strengths or weaknesses. Using a client progress note one is able to gage how the client is progressing.
Medical Progress Note Template
Medical progress note template is done by a medical physician. It is a note or form where all information on a patient’s medical status is recorded during a course of hospitalization or on outpatient. It is an efficient method doctors use for check up on their patients’ progress.
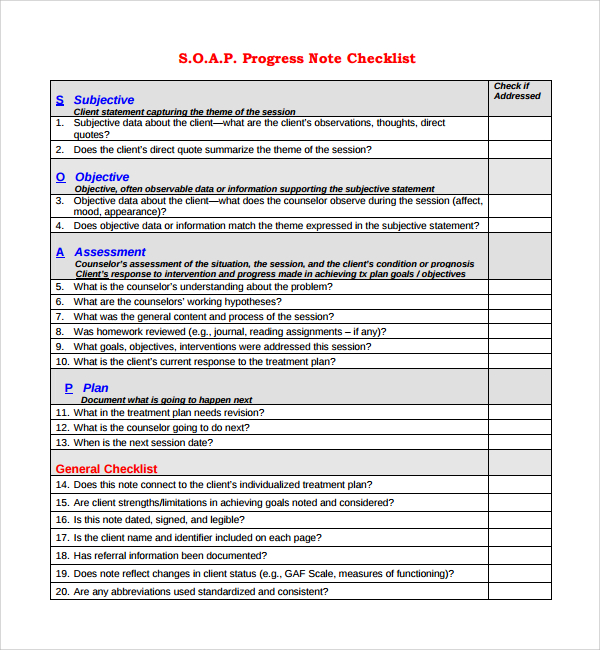
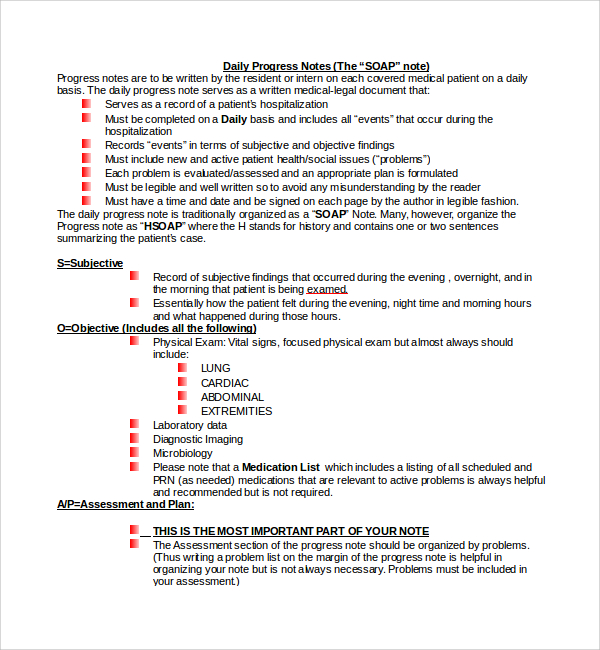
Soap Progress Note Template
The SOAP progress note is a daily medical entry note written by a health physician on each covered medical patient. The Subjective, Objective, Assessment and Plan note summarises a patients’ case.
Baseline Progress Note Template
Electronic progress note Template
Progress Note Template
Free Progress Note Template
Example of Progress Note Template
Printable Progress Note Template
Uses and Purpose of Progress Note Template
Progress note template provides the basis of communication between health care providers on a patient and also enables efficient planning of patient care. Using a progress note template among health providers assist in protecting legal interest of the patient and themselves. It also provides documentation of the care and services received by patient. You can also see Demand Promissory Note
When is a Progress Note Template Issued and For How Long is it Valid?
A progress note template has become a mandatory part of any patient file. A doctor or nurse will most likely issue a progress template note for all patients they attend to or visit the premise. Both short term and long term patients have a progress note written on their medical status. Progress notes are kept valid for the longest time under the medical records. Actually it can be said it stays relevant until the patient is cured but is still kept for future references. You can also see Cornell Notes Paper Template
How to Create / Write a Progress Note Template
A progress note template is a simple note with majorly patient’s information and the doctors notes. Most progress templates follow the SOAP format in writing. SOAP format includes;
Subjective: Subjective describes the patient’s current condition or reason for hospitalization. These are verbally expressed symptoms by the patient themselves or a close party. This can include nausea, cold, swelling inclusive of other descriptions.
Objective: Objective observations include measurable, heard, seen, felt, smelt symptoms. This includes signs like temperature, swelling, pulse and diagnostic results.
Assessment: Assessment is patient’s condition diagnosis. Here several or single clear diagnosis may be made.
Plan: Plan section includes tests ordered, medication prescribed, treatments performed, patient’s disposition, referrals and follow up directions.
It is by far noted the efficiency of progress notes template. Though designed for different uses they are all geared towards the same purpose; efficient patient care. Therefore apply our effective progress templates for your clinical duties and keep your patients well cared for.
If you have any DMCA issues on this post, please contact us!
Related Posts
FREE 14+ Money Promissory Note Samples in PDF
FREE 10+ Thank You Notes For Coworkers Samples in PDF
FREE 10+ Meeting Notes Samples in PDF
FREE 9+ Inpatient Progress Note Samples [ Psychiatric, Hospital, Complaint ]
FREE 10+ Note Taking Samples in PDF
FREE 10+ Credit and Debit Note Samples in PDF | MS Word
FREE 3+ Comprehensive Soap Note Samples in PDF
FREE 8+ Student SOAP Note Samples [ Medical, Pharmacy, Doctor ]
FREE 10+ Return Delivery Note Samples [ Product, Service, Electronic ]
FREE 3+ Car Sale Delivery Note Samples [ Transfer, Private, Vehicle ]
FREE 6+ Goods Delivery Note Samples [ Vehicle, Movement, Return ]
FREE 10+ Doctors Excuse Note Samples [ Office, Visit, Medical ]
FREE 5+ Discharge Summary Nursing Note Samples [ Progress, Patient, Home ]
FREE 6+ Labor and Delivery Note Samples [ Nurse, Progress, Admission ]
FREE 8+ Company Delivery Note Samples in PDF | DOC