The SOAP is a well-known template used by healthcare providers to document sessions or evaluations with their patients. The SOAP note is written proof of what the physician did and observed from their patients. This is important to use as a reference for both physicians and patients for treatment, reference for other healthcare workers when they work together with the physician or take over where someone else left off, documentation for insurance reimbursement, and even use as evidence for court proceedings when things go awry. Since a SOAP note is a powerful document and has many uses, it needs to be written accurately and clearly, so it is easy to follow. This article will guide you on how to write a SOAP note.
8+ Student SOAP Note Samples
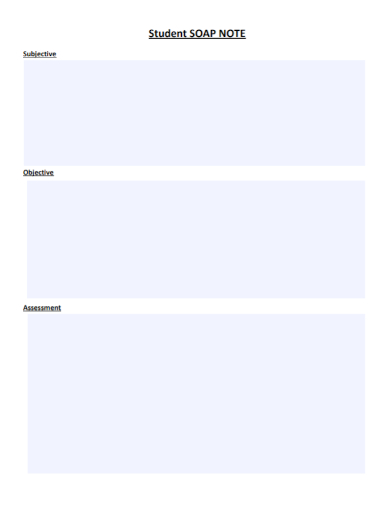
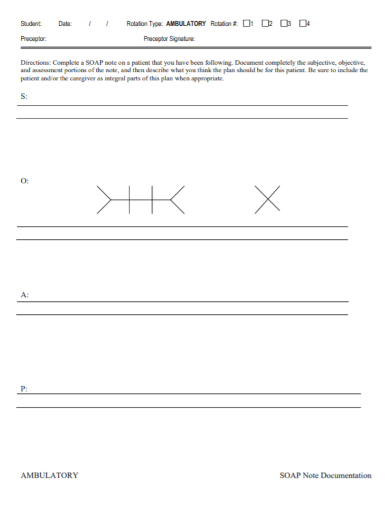
1. Student SOAP Note
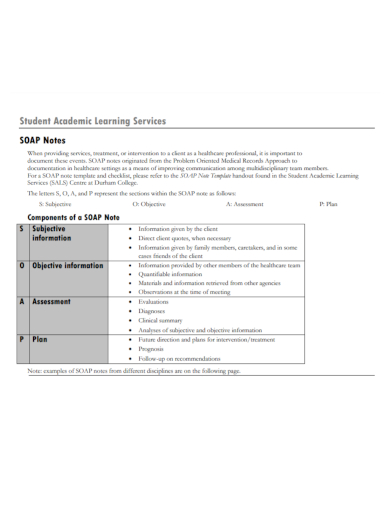
2. Student Academic SOAP Note
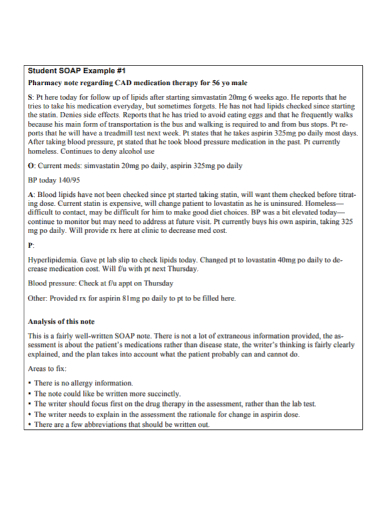
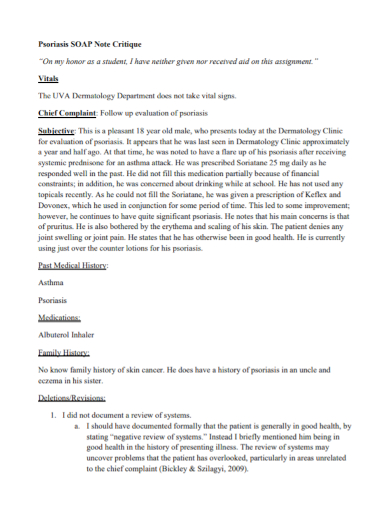
3. Pharmacy Student SOAP Note
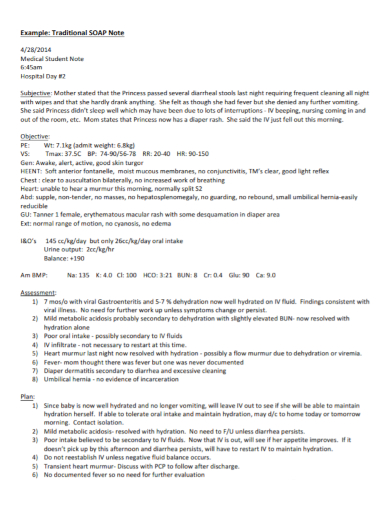
4. Medical Student SOAP Note
5. Student SOAP Documentation Note
6. Student Medication SOAP Note
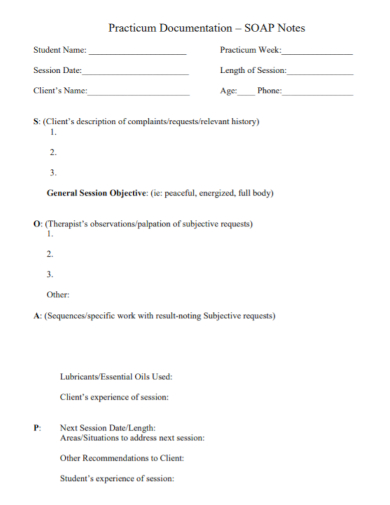
7. Practicum Student SOAP Note
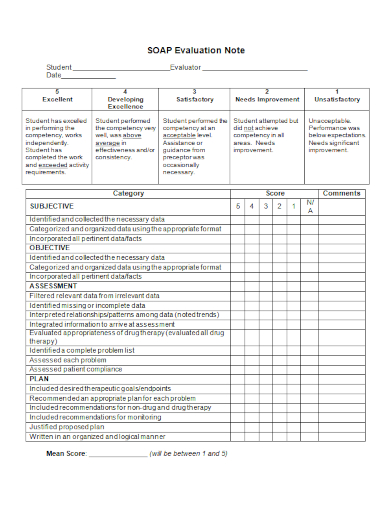
8. Student SOAP Evaluation Note
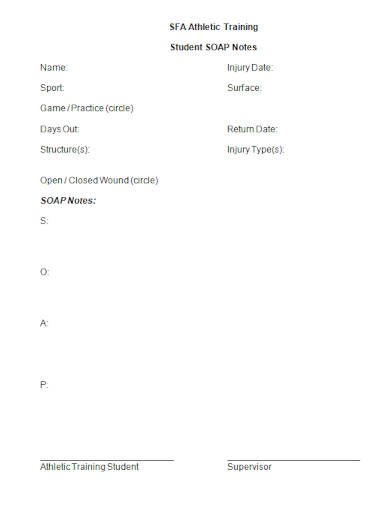
9. Athletic Training Student SOAP Note
What is a SOAP Note?
A SOAP note is a written document that contains specific information about a patient and important aspects of the clinical session with a physician. It includes a statement about the client’s behaviors or status (Subjective), observable and measurable data of the patient from the tests done (Objective), analysis done by the physician of the information given by the client (Assessment), and an outline of the next course of action (Planning). The SOAP note is kept in a patient’s medical record.
Below is more detailed information about the acronyms of the SOAP note:
- (S)Subjective: This is where you will find the statement about relevant client behavior or status such as their complaints or problems they are dealing such as personal or medical issues that are making an impact in their daily routine. This section must contain a complete account of the patient’s symptoms description.
- (O)Objective: This is where you include the factual documentation about the patient such as their diagnosis, and the physician’s observation on their behavioral and/or physical symptoms, appearance, verbal and non-verbal way of communication, body posture, and mood. This is best observed after the physician and client discuss certain topics or issues.
- (A)Assessment: Based on the acquired knowledge from the S and O section, this is where the physician will interpret the information given by the client during the session by implementing their clinical knowledge and understanding.
- (P) Planning: This is where the physician will outline the next course of action as far as the treatment plan goes. The plan should be agreed upon by both the physician and the client. The information will focus on the progression or regression the patient has made in treatment and the nutritional, physical, medical attributes that will contribute to the client’s therapeutic goals. The plan must align with the assessment.
How to Write a SOAP Note
- Start the SOAP note by writing the date and time on the top, left-hand corner of the note.
- In the header, identify where the SOAP note is coming from. This helps the reader locate the note if they want to refer to it later.
- Still at the header, start the note where you will identify the patient’s sex and age, the reason for your interaction with the patient, and the condition/s for which the patient is seeking or receiving therapy.
- Even though you gathered a lot of information from the patient’s interview for the S portion or found information based on the tests done for the O portion, include only information that is relevant and connected to the problem/s being assessed.
- Number each separate medication-related issue in the assessment and use it in the plan.
- Sign the bottom of the SOAP note and place your credentials after your name. Print your name and sign the bottom of the SOAP note. Include your credentials.
- Let your preceptor co-sign the note. Don’t forget to include the clinic or pharmacy contact number so you can be reached out easily if the reader wants to follow up on the SOAP note.
FAQs
What are some useful tips on writing a SOAP note?
A SOAP note is an important document that health professionals such as physicians and nurses use as their reference when treating patients, so it must be written well. Below are some tips one must follow when they write a SOAP note:
- Consider how the patient is represented by avoiding words that suggest any type of judgment towards the patient
- Avoid using tentative language and absolute words
- Remember to write legibly
- Culturally sensitive use language
- When quoting a client, place the exact words in quotation marks
- Keep your notes short, concise and clear
- You can start writing SOAP notes while you are in the session with a patient. Avoid waiting too long after your session with a client or a patient has ended
How long should a SOAP note be?
A SOAP note should not be more than 1-2 pages long for each session.
Don’t forget to review your notes before sending them to the appropriate person in charge for them to use for their recording purposes. Check the SOAP note if you used correct spelling and grammar and your language is clear and concise. Avoid using slang and odd abbreviations that are not easily understandable. Even though writing SOAP notes can be a long and complex task since you have to be precise in your notes, knowing that your notes can contribute greatly to a better outcome for your patient is a great accomplishment to have. To help you get started making the SOAP notes, download our free sample templates above to use as your guide!
Related Posts
FREE 10+ Nurses Notes Samples in PDF
FREE 10+ Narrative Notes Samples in PDF
FREE 10+ After Interview Thank You Note Samples in PDF
FREE 14+ Money Promissory Note Samples in PDF
FREE 10+ Thank You Notes For Coworkers Samples in PDF
FREE 10+ Meeting Notes Samples in PDF
FREE 9+ Inpatient Progress Note Samples [ Psychiatric, Hospital, Complaint ]
FREE 10+ Note Taking Samples in PDF
FREE 10+ Credit and Debit Note Samples in PDF | MS Word
FREE 3+ Comprehensive Soap Note Samples in PDF
FREE 10+ Return Delivery Note Samples [ Product, Service, Electronic ]
FREE 3+ Car Sale Delivery Note Samples [ Transfer, Private, Vehicle ]
FREE 6+ Goods Delivery Note Samples [ Vehicle, Movement, Return ]
FREE 5+ Discharge Summary Nursing Note Samples [ Progress, Patient, Home ]
FREE 6+ Labor and Delivery Note Samples [ Nurse, Progress, Admission ]