5+ Nursing Discharge Summary Samples
Being on top of your patients is crucial in health care management. Additionally, in health care, proper communications needed to document the patient’s medical history and stay. One of the documents used in hospitals and clinics is the discharge summary. Effective discharge planning can reduce the likelihood of you or even your loved one being readmitted to the hospital, as well as aid in rehabilitation, ensure drugs are ordered and administered correctly, and adequately prepare you to take over their care. Communication, a lack of role definition, and a lack of resources were recognized as three major hurdles to the discharge process. In this article, we provide you with free and ready-to-use samples of Nursing Discharge Summary to help you out! Keep on reading to find out more.
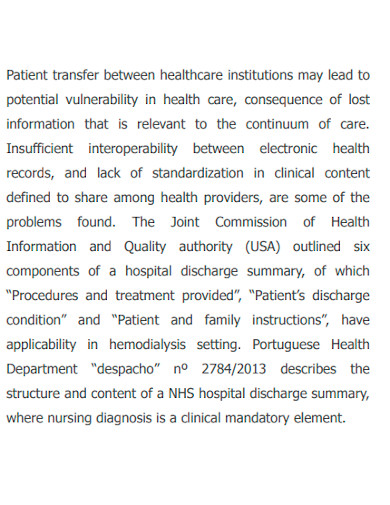
1. Nursing Discharge Summary Sample
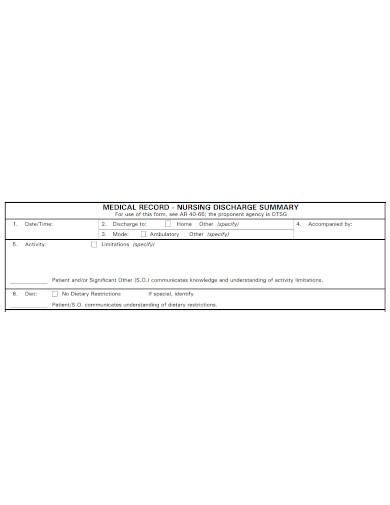
2. Medical Record Nursing Discharge Summary
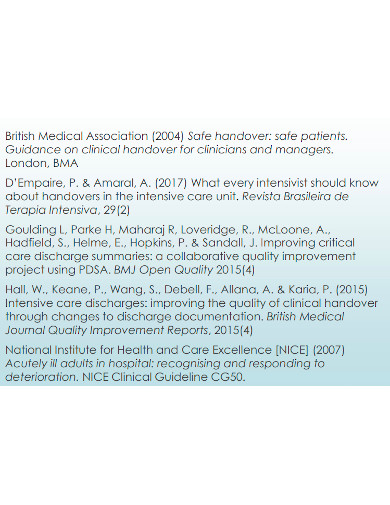
3. Critical Care Nursing Discharge Summary
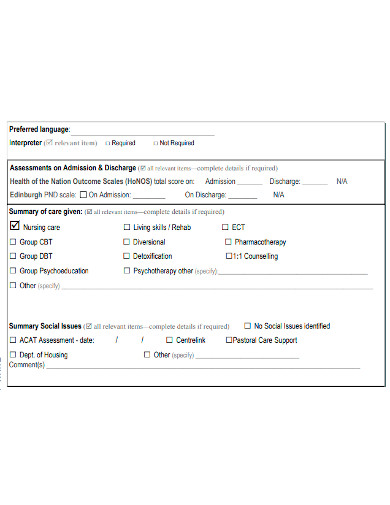
4. Nursing Discharge Summary Form
5. Printable Nursing Discharge Summary
6. Standard Nursing Discharge Summary
What Is a Nursing Discharge Summary?
A discharge summary is a clinical report written by health care experts that explains the specifics of a patient’s hospitalization. The reassessment and evaluation of your nursing care is reflected in discharge summaries. They’re frequently used in conjunction with patient discharge instruction papers, and they provide useful information concerning extra education needs and the patient’s ability to self-care. It is regarded as the major means of communication between the hospital’s medical staff and aftercare providers, emphasizing the need of timely transmission of this document. A Nursing Discharge Summary ensures a smooth and long-lasting transition of the patient to the next level of care, avoiding miscommunication or delays in care that could result in bad results. Poor treatment plans might result from a lack of discharge specifics, diagnosis information, or the patient’s health status in discharge summaries. While a doctor can be the only one to authorize the patient’s release from the hospital, but a nurse can help with the discharge process- which is where the nursing discharge summary comes to light.
How to Make a Discharge Summary
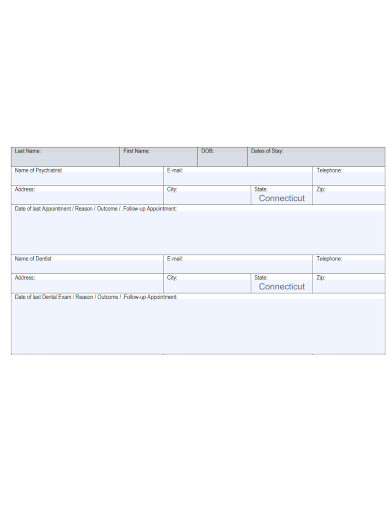
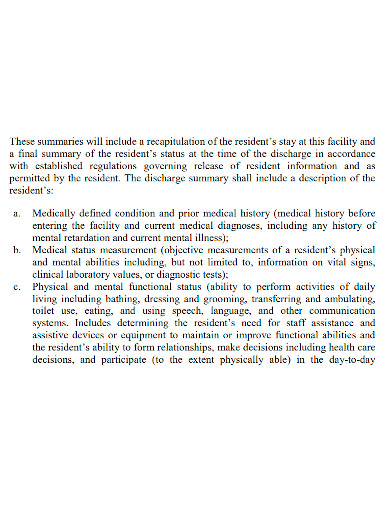
A standard nursing discharge summary includes a recap of a patient’s stay at a hospital, clinic, or other facility, as well as a final summary of the resident’s status at the time of discharge, as permitted by the patient and in accordance with established regulations governing the release of resident information. Aside from the free templates of Nursing Discharge Summaries provided above, you can also try to make one of your own from scratch. To guide you, the discharge summary must include the following information:
1. Client education about the patient, their issues, and their needs.
This specifies the medically defined conditions and prior medical history of the patient. Specifically, the medical history before being admitted to the facility and current medical diagnoses.
2. An explanation of test results and in-hospital procedures, as well as a history of the hospitalization.
This indicates the patient’s physical and mental abilities including, but not limited to, information on vital signs, clinical laboratory values, and diagnostic tests. This is essentially the measurement of the patient’s medical status.
3. Provide the patient’s outstanding issues.
Use this section to communicate what is required to continue providing care such as, the patient’s necessary medication; it’s critical to make a list of all the prescriptions the patient is now taking, as well as those that have been held. Prescription mistakes and bad outcomes might occur if the outpatient medication list is cut and pasted without scrutiny.
4. Include the patient’s mode of discharge.
This heading can be used to indicate whether a patient was released on clinical advise or with clinical consent, whether the patient discharged himself or herself against clinical advice, or whether a relative or advocate discharged the patient.
FAQ
What is the significance of a discharge summary?
Discharge summaries are an important resource that can help patients achieve better results by ensuring continuity of care and a smooth transfer to different settings and providers.
When should you finish a discharge summary?
Unless state law stipulates otherwise, records should be compiled, examined, and finished within 30 days of discharge. Within 24 – 48 hours of discharge, but no more than 72 hours following discharge, a record should be removed from the nursing station.
When should a patient be allowed to leave the hospital?
When you no longer require inpatient treatment and are able to return home, a hospital will discharge you. Alternatively, you may be discharged from a hospital and transferred to another sort of facility. A discharge planner is available in many hospitals.
In conclusion, adopting a structured approach to discharge summaries is crucial in every hospital, clinic, or health care facility. Those who haven’t applied this practice yet, it strongly encouraged to consider adopting this practice. To assist you today, download our free, customized, and printable Nursing Discharge Summaries samples! You can also check out other discharge samples here: Mental Health Discharge Summary, Hospital Discharge Summary, Substance Abuse Discharge plan.
Related Posts
FREE 10+ Consultant Assessment Samples
FREE 9+ Sample Hospital Organizational Chart Templates
FREE 9+ Sample Physical Therapist Job Description Templates
FREE 9+ Sample RN Job Description Templates
FREE 8+ Sample Medical Reports
FREE 8+ Sample Guidance Counselor Resume Templates
FREE 7+ Sample Psychological Evaluation Templates
FREE 7+ Sample New Nurse Resume Templates
FREE 7+ Sample Medical Advice Forms
FREE 5+ Sample Medical Evaluation Templates
FREE 51+ Resume Samples
FREE 23+ Medical Receipt Templates
FREE 9+ Sample DD Form Examples
FREE 9+ Patient Care Technician Job Description Samples
FREE 9+ Sample Clinical Nurse Manager Resumes