Have you ever experienced getting admitted in a hospital? There comes a point where you get better and get cleared from your attending doctor, and when that time comes, the medical staff are given the task to fill out your hospital discharge summary. This task is usually assigned to the junior doctors, and they might have had formal or informal training on how to do this. Are you unsure how to fill up a patient’s hospital discharge summary? Look no further! In this article, we will give some tips to guide you create your own while also providing you with free, downloadable, and editable samples that you could use. Keep on reading!
10+ Hospital Discharge Summary Samples
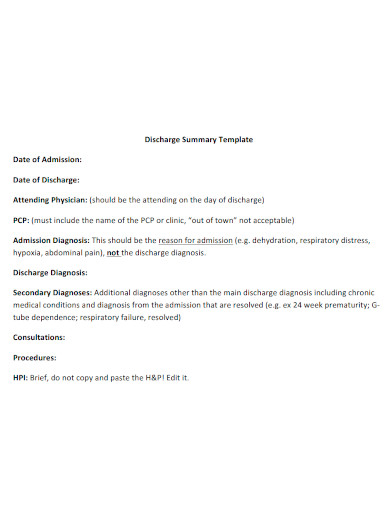
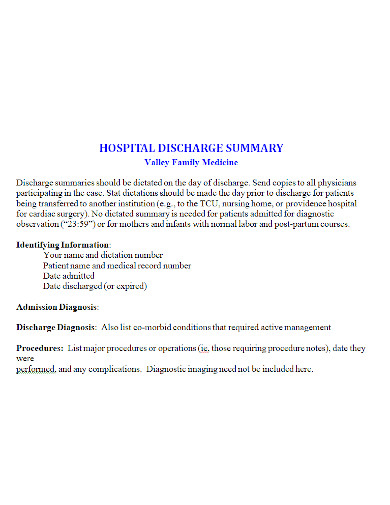
1. Hospital Discharge Summary Sample
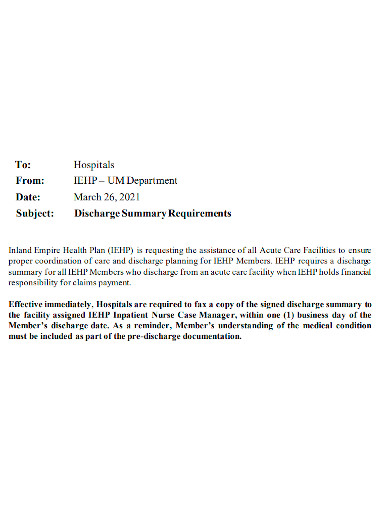
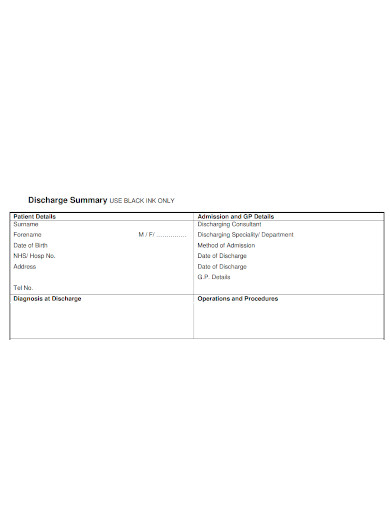
2. Printable Hospital Discharge Summary
3. Hospital Discharge Summary Assessment
4. Standard Hospital Discharge Summary
5. Hospital Discharge Summary Report
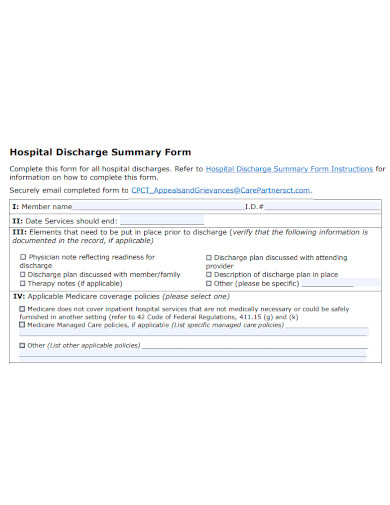
6. Hospital Discharge Summary Form
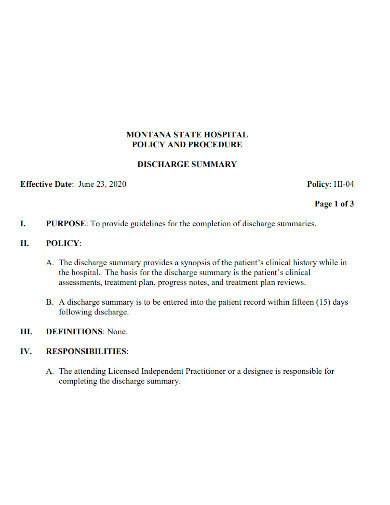
7. Hospital Discharge Summary Policy
8. Editable Hospital Discharge Summary
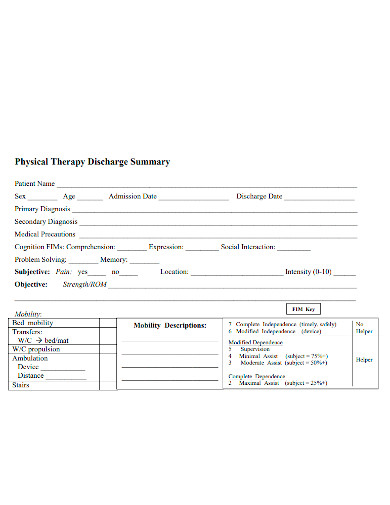
9. Physical Therapy Hospital Discharge Summary
10. Professional Hospital Discharge Summary
11. Hospital Discharge Summary Format
What Is a Hospital Discharge Summary?
According to a report from Advances in Patient Safety, a hospital discharge summary is a ” primary document that function as the means of communicating a patient’s post-hospital care plan to the post-hospital care team. The discharge summary is frequently the only form of communication that the patient receives before moving on to the next level of treatment.” This medical document allows for a secure transition of care from the hospital to the community, offering timely and accurate information to help with ongoing treatment. Therefore, this an important tool in ensuring the safety of patients when they leave the hospital.
How to Create a Hospital Discharge Summary
If you’re interested in creating a hospital discharge summary on your own, here are the key components that this document should contain:
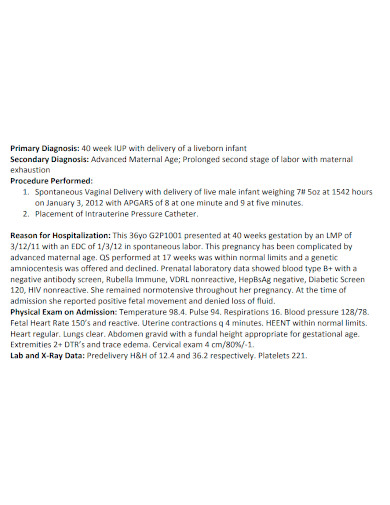
1. Reason for Hospitalization
This should include the patient’s initial condition during the hospital admission, the hospital’s initial diagnostic evaluation, and the patient’s present condition.
2. Significant Findings
This section discloses the primary diagnosis given by the attending physicians to the patient. Simply put, the primary diagnosis is the root cause of the admission. It will shed light on the patient’s main condition that was treated or explored during the relevant healthcare episode; such as the main symptoms and abnormal findings.
3. Instructions for the patient and their family
This section consists of the following:
- discharge medications
- activity orders
- therapy orders
- dietary instructions
- plans for medical follow-up
4. Signature of the attending physician
Most importantly, the signature of the patient’s attending physician is required in order to authenticate the information and instructions reported in the hospital discharge summary. Without it, the document will be considered erroneous.
These are the fundamental that summarizes a hospital discharge summary document. While it serves as a strong foundation for the summary, there are also other components that could be considered to further improve patient safety.
FAQs
What is the importance of a discharge summary?
A discharge summary is a handover document that describes why the patient was hospitalized, what occurred to them while they were in the hospital, and all the information they need to take over the patient’s care swiftly and effectively.
How does hospital discharge work?
The process of leaving a hospital following treatment is known as hospital discharge. When you no longer require inpatient treatment and are able to return home, a hospital will discharge you. Alternatively, you may be discharged from a hospital and transferred to another sort of facility. A discharge planner is available in many hospitals.
What is a discharge summary used for?
A discharge summary is a summary of a patient’s hospital stay from admission to discharge written by a physician. It’s a tool that helps professionals outside the hospital comprehend what happened to the patient while they were in the hospital.
What is a safe hospital discharge?
Hospitals are prohibited from dismissing patients who do not have a safe plan for continuous care after they leave the hospital under the Safe Hospital Discharge laws.
When should a discharge summary be completed?
Unless local law says otherwise, records should be compiled, examined, and finished within 30 days of discharge. Within 24 – 48 hours of discharge, but no more than 72 hours following discharge, a record should be removed from the nursing station.
A Hospital Discharge summary, in essence, ensures the safety of a patient. It gives the necessary information needed to assure the seamless transition of the inpatient healthcare to the outpatient activities required. Hence, with the use of our free templates, you are provided with great examples on how to create a summary that is effective and efficient. Print these samples out and you’re good to go!
Related Posts
FREE 10+ Dog Tag Samples in PDF | MS Word
FREE 5+ User Stories Samples in PDF
FREE 10+ Social Media Audit Samples in PDF | MS Word
FREE 10+ Faculty Self Assessment Samples in PDF
FREE 4+ Job-Sharing Agreement Form Samples in PDF
FREE 10+ Annual Evaluation Form Samples [ Employee, Manager, Performance ]
FREE 9+ Sample Private Contracts in PDF | MS Word
FREE 8+ Sample Prize Competition Rules in PDF
FREE 10+ Inventory Samples (Equipment, Software)
FREE 6+ Book Samples [Recipe, Comic, Address]
FREE 4+ Sample Case Files [Business, CD]
FREE 5+ Message Samples (Holiday, Phone, Welcome)
FREE 4+ Credit Samples (Report, Memo, Note)
FREE 6+ Tutor Employment Contract Samples in PDF | MS Word
FREE 4+ Tutor Consent Form Samples in MS Word | PDF