What is a prior authorization form? When your physician prescribes you a certain medication, laboratory test, or other procedures, they are required to obtain prior authorization from your health insurance company. This process is used as a safety measure and at the same time minimizes the cost that health insurance companies pay. It usually contains your personal information, your provider’s information, medication information, and clinical information.
The terms pre-authorization, pre-certification, and notification are also used in place of prior authorization. Prior authorization forms are the documents used to request for the approval of the medication or procedure. We have prepared Sample Forms that are available for you to view or download online.
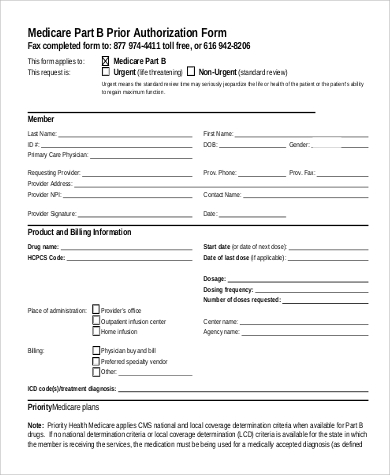
Medicare Prior Authorization Form
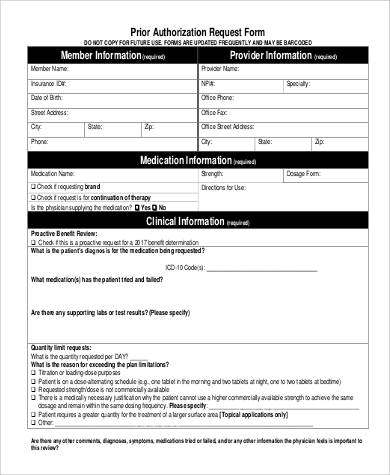
Prior Authorization Request Form
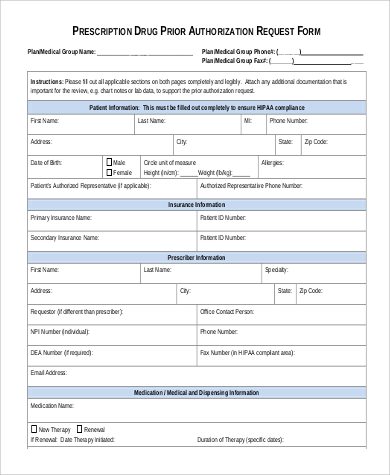
Prescription Prior Authorization Form
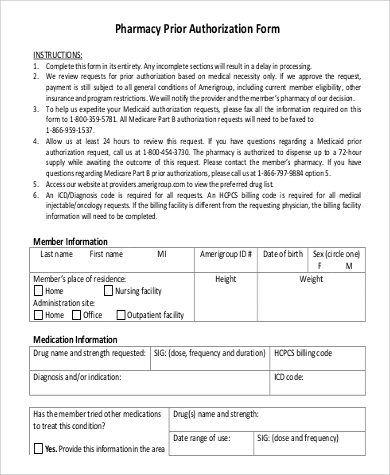
Pharmacy Prior Authorization Form
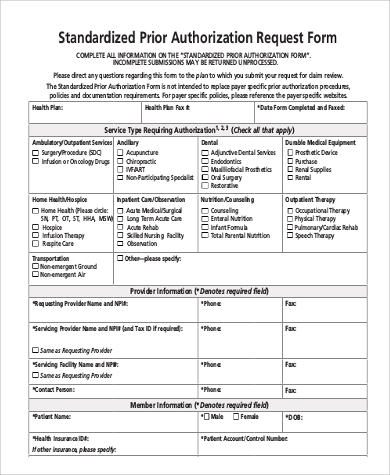
Standardized Prior Authorization Request Form
What Things Require Prior Authorization
Not all physician prescriptions or procedures require prior authorization. The procedures that require prior authorization varies from one health insurance provider to another. To know about the procedures that require prior authorization, you may contact your health insurance provider. Here are some of the procedures or things that require prior authorization:
- magnetic resonance imaging (MRI) and computerized tomography (CT) scan
- hospital admission that are non-emergency or did not come through the emergency department
- air ambulance if available in your area or country
- ground ambulance
- in-patient facilities
- surgeries
- specialty drugs
- transplant services
What Happens If Prior Authorization Is Not Secured?
Failure to obtain a prior authorization form will result to low reimbursements and low benefits for the patient. Sometimes what happens is really up to the health insurance plan provider. It also depends on the agreement signed by the patient upon signing up for the health insurance plan. There are instances where the patient is liable for covering the payment if they seek services that require prior authorization but didn’t obtain one. Insurance providers deny payment of health services that are performed without authorization. The patient may also be asked to cover the payment for the service if that kind of situation happens. You may also want to check the Medicaid Prior Authorization Form.
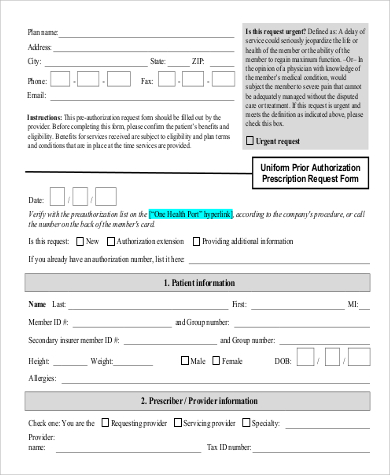
Uniform Prior Authorization Form
Universal Prior Authorization Medication Form
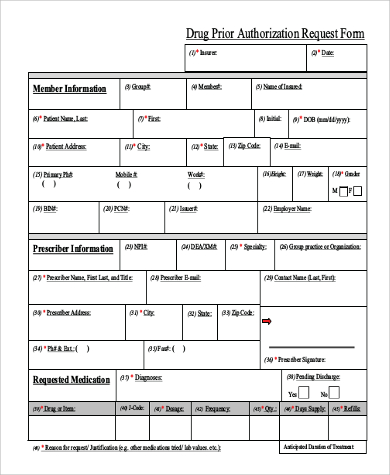
Drug Prior Authorization Request Form
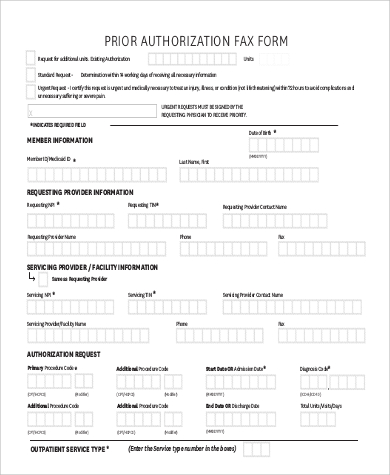
Prior Authorization Fax Form
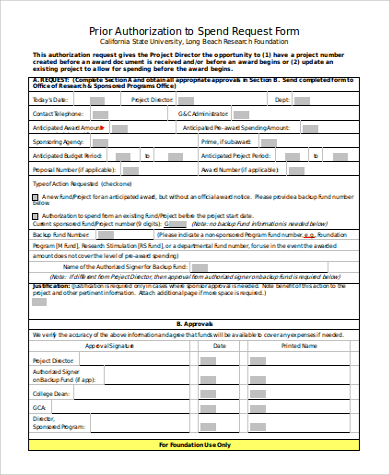
Prior Authorization to Spend Request Form
Advantages of Prior Authorization
- Prevents unnecessary procedures to be done to patients.
- For safety measures. The patient needs to use approved medications or procedures first before the prescribed medication or procedure requested by the health provider is approved.
- It is a cost-saving measure.
- New prescription drugs require prior authorization, thus prevents potential dangerous drug interactions.
Disadvantages of Prior Authorization
- It is time-consuming. Physicians have expressed their frustration about the time they have spent interacting with health insurance providers to obtain authorization.
- It is costly. While prior authorizations can help health insurance providers save costs, it is not the case among physicians, nurses, and clerical staff. If the time they spent interacting with the insurance provider is converted to money, then it is quite costly.
- Physicians or health providers are burdened by obtaining pre-authorizations.
With the availability of prior authorization forms online, there will be no reason for you not to be able to acquire one. It is best that you download our sample prior authorization forms or the Sample Caremark Prior Authorization Form. It is a valuable tool that can be used to obtain pre-authorization from health insurance providers. You don’t have to think about what to put in, simply fill in the blanks or boxes with the required information and you are good to go. It is that easy and convenient. So don’t leave without downloading.
Related Posts
Agreement Form Samples & Templates
Vehicle Inspection Forms Samples & Templates
Sample Employee Advance Forms
Sample Child Travel Consent Forms
Sample Testimonial Request Forms
Sample Employee Details Forms
Sample Divorce Forms
Sample Attestation Forms
Employee Performance Appraisal Form Templates
FREE 9+ Sample Presentation Evaluation Forms in MS Word
FREE 10+ School Admission Form Samples & Templates in MS Word | PDF
FREE 30+ Patient Consent Form Samples in PDF | MS Word
FREE 10+ Sample Sign Off Form Templates in PDF | MS Word
FREE 11+ Sample Medical Consultation Forms in PDF | MS Word
FREE 8+ Sample Donation Forms in PDF | MS Word